
WIC
Participation
and
Pregnancy
Outcomes:
Massachusetts
Statewide
Evaluation
Project
MILTON
KOTELCHUCK,
PHD,
MPH,
JANET
B.
SCHWARTZ,
MS,
RD,
MARLENE
T.
ANDERKA,
MPH,
AND
KARL
S.
FINISON,
MA
Abstract:
The
effects
of
WIC
prenatal
participation
were
exam-
ined
using
data
from
the
Massachusetts
Birth
and
Death
Registry.
The
birth
outcomes
of
4,126
pregnant
women
who
participated
in
the
WIC
program
and
gave
birth
in
1978
were
compared
to
those
of
4,126
women
individually
matched
on
maternal
age,
race,
parity,
education,
and
marital
status
who
did
not
participate
in
WIC.
WIC
prenatal
participants
are
at
greater
demographic
risk
for
poor
pregnancy
outcomes
compare
to
all
women
in
the
same
community.
WIC
participation
is
associated
with
improved
pregnancy
outcomes,
including,
a
decrease
in
low
birthweight
(LBW)
incidence
(6.9
per
cent
vs
8.7
per
cent)
and
neonatal
mortality
(12
vs
35
deaths),
an
Introduction
Efforts
to
improve
the
health
status
of
pregnant
women
and
their
young
children
through
nutritional
supplementa-
tion
and
education
have
long
been
a
part
of
public
health
programs
in
the
United
States.
The
Special
Supplemental
Food
Program
for
Women,
Infants
and
Children
(WIC),
established
in
1972,
is
the
largest
and
most
specifically
targeted
public
health
nutrition
program
in
the
United
States
today.
The
WIC
program
is
designed
to
reach
high-risk
pregnant
and
lactating
women,
infants,
and
children
up
to
5
years
of
age
with
supplemental
foods
and
nutrition
educa-
tion,
as
an
adjunct
to
good
health
care.'
WIC
is
the
first
federal
nutrition
program
to
use
identifi-
able
nutritional
risk,
in
addition
to
low
income,
as
a
criterion
for
eligibility.
Since
its
inception,
WIC
has
grown
to
provide
benefits
to
2.9
million
persons
monthly,
at
a
cost
of
$1.36
billion
in
fiscal
year
1983.
An
estimated
500,000
pregnant
women
now
participate
in
the
WIC
program.
Eligible
participants
receive
a
monthly
set
of
food
vouchers
redeemable
at
local
grocers
for
specific
foods
tailored
to
individual
needs.
Allowable
foods
include:
milk,
cheese,
iron-fortified
cereal,
100%
fruit
juices,
eggs,
dried
beans,
peanut
butter,
and
iron-fortified
formula
for
infants.
The
cost
of
the
food
package
is
approximately
$30
per
month,
provided
at
no
cost
to
the
participants.
Nutrition
education
is
also
provided.
A
more
complete
description
of
the
WIC
program
appears
elsewhere.2
The
WIC
program,
despite
its
magnitude
and
its
clearly
stated
public
health
goals,
has
not
been
extensively
exam-
ined.
The
lack
of
research
may
be
the
result
of
a
moral
acceptance
of
the
virtues
of
feeding
high-risk
women
or
of
the
methodological
difficulties
of
conducting
quality
re-
search
in
a
large,
decentralized
nutrition
program.
The
latter
include
the
difficulty
of
obtaining
a
proper
comparison
sample,
the
lack
of
data
collected
uniformly
across
program
sites,
and
the
need
for
large
sample
sizes
to
show
stable
From
the
Division
of
Family
Health
Services,
Massachusetts
Department
of
Public
Health.
Address
reprint
requests
to
Milton
Kotelchuck,
PhD,
MPH,
Department
of
Social
Medicine
and
Health
Policy,
Harvard
Medical
School,
25
Shattuck
Street,
Boston,
MA
02115.
This
paper,
submitted
to
the
Journal
June
27,
1983,
was
revised
and
accepted
for
publication
March
21,
1984.
Editor's
Note:
See
also
Different
Views,
pp
1145-1149
this
issue.
C
1984
American
Journal
of
Public
Health
0090-0036/84
$1.50
increase
in
gestational
age
(40.0
vs
39.7
weeks),
and
a
reduction
in
inadequate
prenatal
care
(3.8
per
cent
vs
7.0
per
cent).
Stratification
by
demographic
subpopulations
indicates
that
subpopulations
at
higher
risk
(teenage,
unmarried,
and
Hispanic
origin
women)
have
more
enhanced
pregnancy
outcomes
associated
with
WIC
participa-
tion.
Stratification
by
duration
of
participation
indicates
that
in-
creased
participation
is
associated
with
enhanced
pregnancy
out-
comes.
While
these
findings
suggest
that
birth
outcome
differences
are
a
function
of
WIC
participation,
other
factors
which
might
distinguish
between
the
two
groups
could
also
serve
as
the
basis
for
alternative
explanations.
(Am
J
Public
Health
1984;
74:1086-1092.)
program
effects.
To
date,
only
two
evaluations
of
prenatal
participation
in
WIC
based
on
perinatal
outcomes
have
been
published.
Despite
quite
divergent
methodologies,
Edozien,
et
al,3
and
Kennedy,
et
al,4
both
reported
that
WIC
partici-
pation
is
positively
associated
with
maternal
weight
gain,
infant
birthweight,
and
gestational
age,
and
that
the
WIC
programs'
effectiveness
is
enhanced
by
increasing
duration
of
participation.
Others
maintain
that
the
value
of
WIC
is
unproven.5
This
paper
reports
the
results
of
the
Massachusetts
WIC
Statewide
Evaluation
Project,
which
examined
the
associa-
tion
between
maternal
participation
in
the
WIC
Program
in
1978
and
the
outcomes
of
pregnancy.
Specifically,
four
questions
were
addressed:
*
Does
the
WIC
Program
reach
its
target
population?
*
Is
WIC
participation
associated
with
more
positive
outcomes
of
pregnancy?
*
Are
the
effects
of
WIC
participation
similar
across
all
high-risk
subpopulations?
*
Are
the
effects
of
the
WIC
program
enhanced
with
increased
duration
of
participation?
The
Massachusetts
WIC
Program
The
Massachusetts
WIC
program
is
similar
to
WIC
programs
nationally.
In
1978,
it
operated
through
23
non-
profit
local
health
centers
and
social
service
agencies
under
contract
with
the
State
Department
of
Public
Health.
Ap-
proximately
22,000
persons
participated
monthly,
of
whom
over
4,000
were
pregnant
women.
At
the
time
of
the
study,
geographic
eligibility,
in
addition
to
income
guidelines
and
nutritional
risk,
was
a
criterion
for
WIC
participation.
In
Massachusetts,
the
issuance
and
redemption
of
all
WIC
food
vouchers
is
centrally
monitored
through
a
single
computerized
bank
control
system.
This
system
allows
for
an
accurate
documentation
of
the
names,
duration
of
partici-
pation,
and
number
of
vouchers
redeemed
for
all
prenatal
WIC
participants.
Methodology
Study
Population
The
basic
design
of
the
study
is
a
direct
comparison
of
the
pregnancy
outcomes
of
two
groups
of
Massachusetts
women
who
gave
birth
in
1978:
those
who
participated
in
the
WIC
prenatal
program,
and
a
matched
control
group
of
non-
WIC
women.
The
derivation
of
the
study
population
and
AJPH
October
1984,
Vol.
74,
No.
10
1086
WIC
PARTICIPATION,
PREGNANCY
OUTCOME:
MASSACHUSETTS
TABLE
1-Selected
Maternal
Demographic
Characteristics,
1978:
WIC
Participants,
Catchment
Area
Resi-
dents
and
All
Massachusetts
Residents
%
WIC
%
Catchment
%
All
Massachusetts
%
WIC
Saturation
Characteristics
Participants
Area
Residents
Residents
of
Catchment
Area
Age
s17
years
12.2
6.0
3.8
36.4
l19
years
28.6
16.9
11.5
30.4
Education
-9
years
14.9
10.5
5.1
25.4
<12
years
49.2
31.5
19.0
28.0
Mantal
Status
Unmarried
40.7
23.9
13.7
30.6
Married
59.3
76.1
86.3
14.0
Race
Black
23.8
16.0
6.2
27.0
White
73.6 81.6
91.8
16.2
Parity
1
44.9 45.9
44.6
17.6
5+
6.5
4.1
3.3
28.4
TOTAL
(N)
(4,126)
(22,995)
(67,187)
study
data
results
from
the
linkage
of
two
computerized
data
systems:
the
WIC
bank
voucher
system,
and
the
State
Birth
and
Death
Registry.
Appendix
A
summarizes
the
three
steps
were
involved.*
First,
the
names
of
all
women
who
registered
as
a
WIC
prenatal
participant
were
drawn
from
the
WIC
computerized
participant
voucher
reports
(N
=
4,898).
Data
on
the
dura-
tion
and
number
of
vouchers
cashed
per
month
were
also
extracted.
Failure
to
pick
up
vouchers
for
two
consecutive
months
resulted
in
administrative
termination
from
the
pro-
gram.
Administrative
termination
codes
were
noted
on
525
names.
Specific
causes
for
termination
were
known
for
172
of
the
names,
while
353
names
remained
unaccounted
for.
As
this
was
a
study of
women
who
actively
participated
in
WIC,
all
525
women
with
termination
codes
were
excluded
from
the
study,
leaving
4,373
eligible
participants.
Second,
each
mother's
name
(plus
town
of
residence,
race,
and
expected
date
of
delivery)
obtained
from
the
WIC
reports
was
linked,
by
hand,
to
the
corresponding
infant's
birth
certificate
record
listed
in
the
state's
computerized
Birth
Registry
file.
Twin
births
(46)
and
know
fetal
deaths
(15)
were
excluded,
as
were
191
names
which
could
not
be
positively
linked.
Third,
each
WIC
participant
was
individually
matched
to
a
control
subject
on
the
basis
of
five
maternal
characteris-
tics
available
on
the
birth
certificates:
age,
race,
parity,
educational
level,
and
marital
status
(Appendix
B).
Controls
were
selected
from
the
pool
of
64,000
remaining
non-WIC
births
in
the
computerized
State
Birth
Registry
(68,000
total
1978
resident
births
minus
the
approximately
4,000
WIC
births).
Matching
was
performed
by
hand
with
the
aid
of
computer-derived
lists.
Efforts
were
made
to
facilitate
geo-
graphic
similarity
of
the
WIC
and
control
populations;
matching
was
attempted
first
within
the
same
catchment
area,
then
within
similar
types
of
towns,
and
finally
any-
where
within
the
state.
The
first
eligible
woman
meeting
all
five
study
criteria
was
chosen.
All
matching
was
exact.**
Five
subjects
who
could
not
be
matched
were
excluded.
The
final
sample,
composed
of
4,126
matched
pairs
of
*
Detailed
procedure
manual
available
from
authors
upon
request.
**
Since
the
computerized
birth
registry
is
sequenced
by
date
of
birth,
the
control
subjects
tend
to
be
bom
earlier
in
the
year.
Given
the
expansion
of
the
WIC
program
in
Massachusetts
during
1978,
the
WIC
subjects
tend
to
be
born
later
in
the
year.
No
seasonality
bias
in
birth
outcomes
was
noticed.
WIC
and
non-WIC
mothers,
included
95
per
cent
of
all
eligible
1978
prenatal
WIC
participants
in
Massachusetts.
Derivation
of
Study
Data
Once
the
WIC
cases
and
matched
controls
were
select-
ed,
all
data
from
their
birth
certificates
were
extracted
for
analysis.
The
Massachusetts
birth
certificate
provides
data
on
maternal
demographic
characteristics,
prenatal
care,
and
pregnancy
outcomes.6
The
State
Death
Registry
file
pro-
vides
information
on
all
neonatal
deaths
between
birth
and
28
days.
Data
Analysis
The
demographic
characteristics
of
WIC
participants
were
contrasted
with
the
characteristics
of
all
pregnant
women
residing
in
the
same
catchment
area
and
statewide
in
1978.
WIC
participants
were
then
compared
directly
to
their
matched
non-WIC
controls
on
the
birth
outcome
measures.
Differences
were
statistically
examined
by
use
of
paired
T-
test
comparisons
for
continuous
data
items
and
by
McNemar
Chi-square
comparisons
for
ordinal
data
items.
Pairwise
deletions
were
used
for
any
subject
pair
having
missing
data.
The
women
in
the
WIC
sample
and
their
matched
controls
were
then
stratified
into
a
number
of
subpopulations
for
separate
analyses
of
birth
outcome
differences.
These
sub-
groups
were
defined
on
the
basis
of
demographic
character-
istics
or
duration
of
WIC
participation
and
are
not
statistical-
ly
independent
of
each
other.
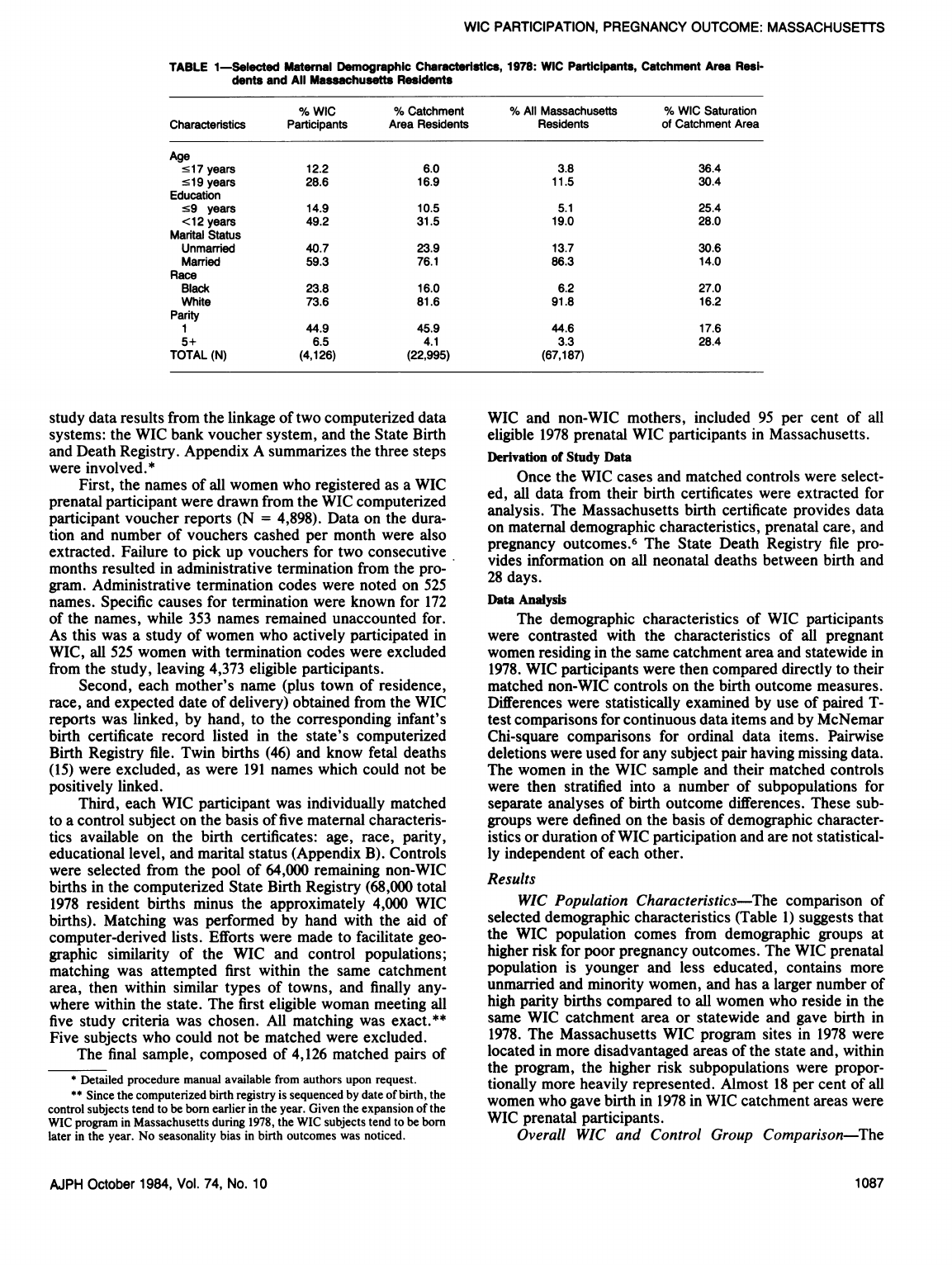
Results
WIC
Population
Characteristics-The
comparison
of
selected
demographic
characteristics
(Table
1)
suggests
that
the
WIC
population
comes
from
demographic
groups
at
higher
risk
for
poor
pregnancy
outcomes.
The
WIC
prenatal
population
is
younger
and
less
educated,
contains
more
unmarried
and
minority
women,
and
has
a
larger
number
of
high
parity
births
compared
to
all
women
who
reside
in
the
same
WIC
catchment
area
or
statewide
and
gave
birth
in
1978.
The
Massachusetts
WIC
program
sites
in
1978
were
located
in
more
disadvantaged
areas
of
the
state
and,
within
the
program,
the
higher
risk
subpopulations
were
propor-
tionally
more
heavily
represented.
Almost
18
per
cent
of
all
women
who
gave
birth
in
1978
in
WIC
catchment
areas
were
WIC
prenatal
participants.
Overall
WIC
and
Control
Group
Comparison-The
AJPH
October
1984,
Vol.
74,
No.
10
1087
KOTELCHUCK,
ET
AL.
TABLE
2-Comparlson
of
WIC
and
Control
Birth
Outcomes
95%
Confidence
Findings
N
WiC
Control
Difference
Interval
Birthweight
Birthweight
(in
grams)
4121
3281
3260
+210
t23.4
Per
Cent
Low
Birthweight
4121
6.9
8.7
-1.8**
±1.1
Per
Cent
Small
for
Gestational
Aget
3615
5.0
5.0
0.0
±1.0
Gestation
Adjusted
Birthweight
(in
grams)tt
4121
-52.0 -48.4
-3.6
±21.9
Gestation
Gestational
Age
(in
weeks)
3722
40.0
39.7
+0.3***
+.1
Per
Cent
Premature
(<37
weeks)
3722
8.5
9.8
-1.3'
±1.3
Morbidity
Per
Cent
with
Complications
of
Pregnancy,
Delivery
and
Labor
4115
20.2
21.1
-0.9
±1.7
Per
Cent
with
Congenital
Malformations
4126
1.7
1.7
0.0
±0.6
Per
Cent
Low
(<5)
Apgar
Score
(one
minute)
3732
5.1
5.7
-0.6
±1.0
Per
Cent
Low
(<5)
Apgar
Score
(five
minute)
3716
.5
1.0
-0.5*
±0.4
Mortality
Number
of
Neonatal
Deaths
4126
12
35
-23**
+13
Prenatal
Care
Number
of
Prenatal
Visits
3721
11.2
10.8
+0.4***
±0.2
Month
Prenatal
Care
Began
3721
2.7
2.9
-0.2***
±0.1
Adequacy
of
Prenatal
Care
indexttt
3675
1.34
1.41
-0.07***
±0.03
Per
Cent
with
Inadequate
Care
-
3.9
7.0
-3.1"'
±1.0
Per
Cent
with
Intermediate
Care
-
26.7
26.7
0.0
±2.0
Per
Cent
with
Adequate
Care
-
69.4
66.3
+3.1"
±2.1
0
p
<
.10.
=
p
<
.05.
=p
<.01.
=p
<
.001.
tSmall
for
gestational
ages
is
defined
as
an
infant
weighing
below
the
1
0th
percentile
for
their
gestational
age
at
birth.
Figures
derived
from
Battaglia
and
Lubchecno.7
ttThe
gestational
correction
for
birthweight
is
determined
by
subtracting
the
observed
birthweight
from
the
mean
Massachusetts
birthweight
for
that
gestational
age.
tttThe
Institute
of
Medicine
adequacy
of
prenatal
care
index
is
a
3-point
index
combining
the
number
of
prenatal
visits
and
month
prenatal
care
began,
with
an
adjustment
for
gestational
age.
Adequate
care
assumes
that
the
first
prenatal
care
visit
occurs
in
1st
trimester,
with
one
additional
visit
per
month
of
pregnancy.8
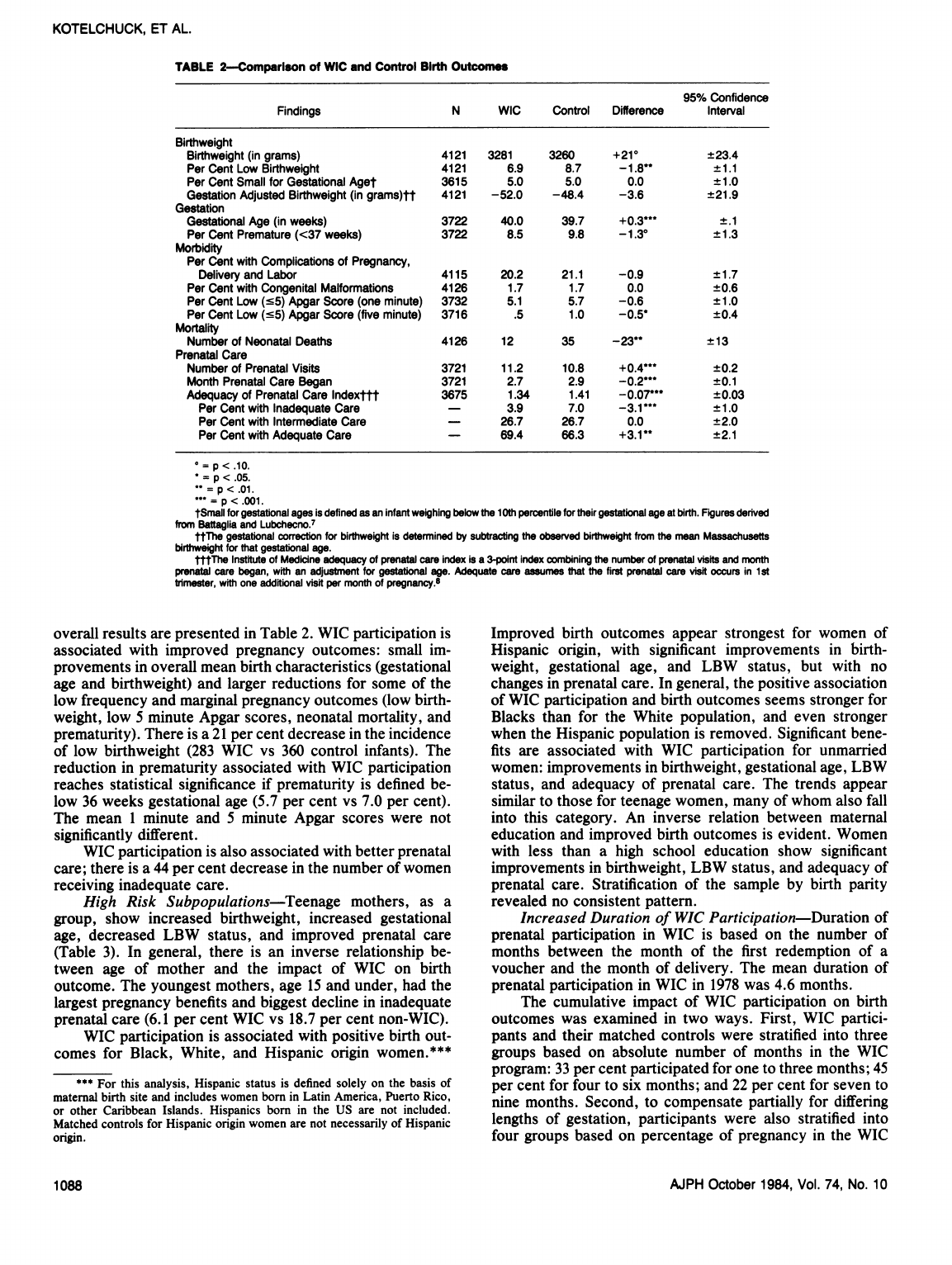
overall
results
are
presented
in
Table
2.
WIC
participation
is
associated
with
improved
pregnancy
outcomes:
small
im-
provements
in
overall
mean
birth
characteristics
(gestational
age
and
birthweight)
and
larger
reductions
for
some
of
the
low
frequency
and
marginal
pregnancy
outcomes
(low
birth-
weight,
low
5
minute
Apgar
scores,
neonatal
mortality,
and
prematurity).
There
is
a
21
per
cent
decrease
in
the
incidence
of
low
birthweight
(283
WIC
vs
360
control
infants).
The
reduction
in
prematurity
associated
with
WIC
participation
reaches
statistical
significance
if
prematurity
is
defined
be-
low
36
weeks
gestational
age
(5.7
per
cent
vs
7.0
per
cent).
The
mean
1
minute
and
5
minute
Apgar
scores
were
not
significantly
different.
WIC
participation
is
also
associated
with
better
prenatal
care;
there
is
a
44
per
cent
decrease
in
the
number
of
women
receiving
inadequate
care.
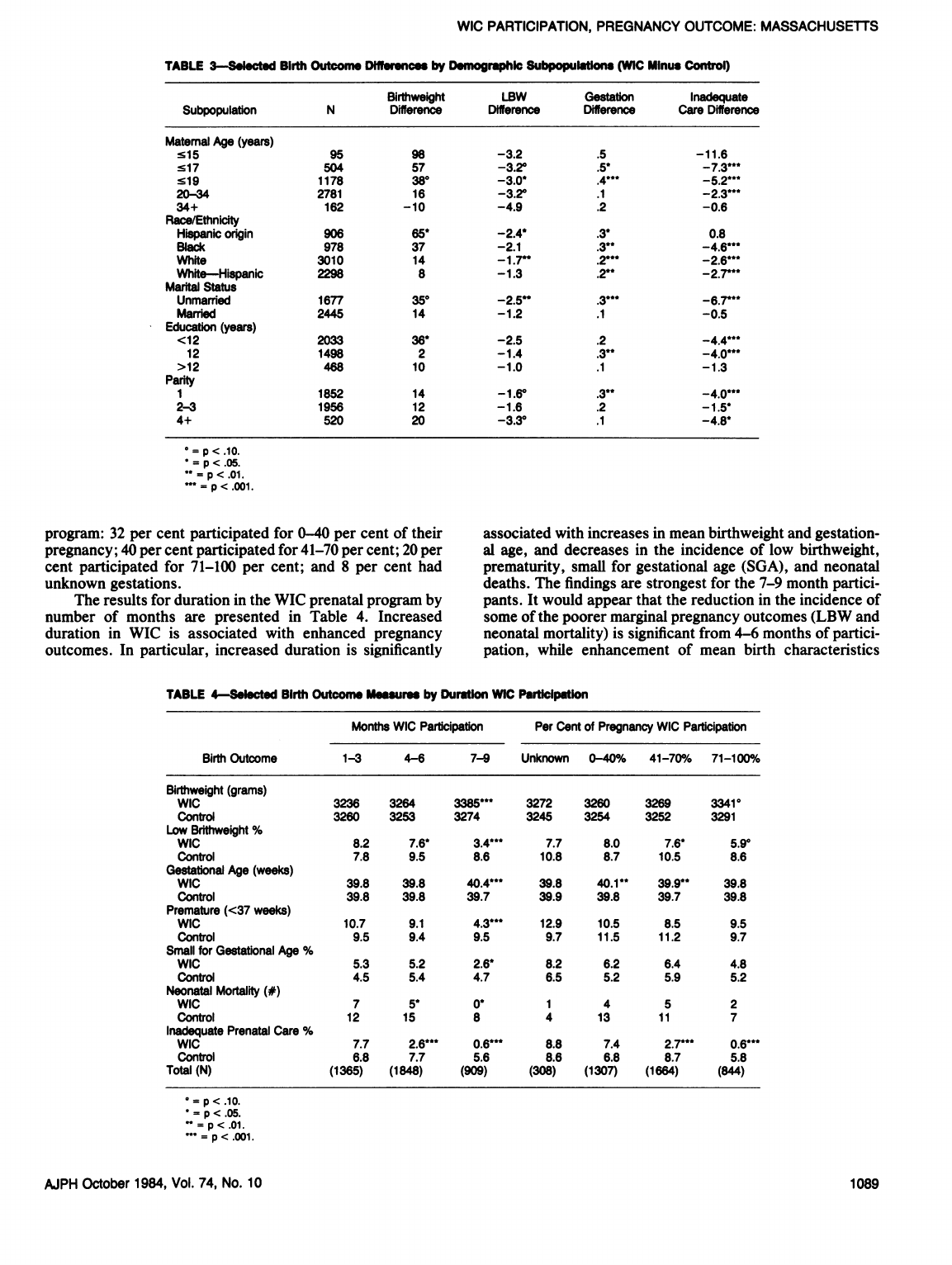
High
Risk
Subpopulations-Teenage
mothers,
as
a
group,
show
increased
birthweight,
increased
gestational
age,
decreased
LBW
status,
and
improved
prenatal
care
(Table
3).
In
general,
there
is
an
inverse
relationship
be-
tween
age
of
mother
and
the
impact
of
WIC
on
birth
outcome.
The
youngest
mothers,
age
15
and
under,
had
the
largest
pregnancy
benefits
and
biggest
decline
in
inadequate
prenatal
care
(6.1
per
cent
WIC
vs
18.7
per
cent
non-WIC).
WIC
participation
is
associated
with
positive
birth
out-
comes
for
Black,
White,
and
Hispanic
origin
women.***
***
For
this
analysis,
Hispanic
status
is
defined
solely
on
the
basis
of
maternal
birth
site
and
includes
women
born
in
Latin
America,
Puerto
Rico,
or
other
Caribbean
Islands.
Hispanics
born
in
the
US
are
not
included.
Matched
controls
for
Hispanic
origin
women
are
not
necessarily
of
Hispanic
origin.
Improved
birth
outcomes
appear
strongest
for
women
of
Hispanic
origin,
with
significant
improvements
in
birth-
weight,
gestational
age,
and
LBW
status,
but
with
no
changes
in
prenatal
care.
In
general,
the
positive
association
of
WIC
participation
and
birth
outcomes
seems
stronger
for
Blacks
than
for
the
White
population,
and
even
stronger
when
the
Hispanic
population
is
removed.
Significant
bene-
fits
are
associated
with
WIC
participation
for
unmarried
women:
improvements
in
birthweight,
gestational
age,
LBW
status,
and
adequacy
of
prenatal
care.
The
trends
appear
similar
to
those
for
teenage
women,
many
of
whom
also
fall
into
this
category.
An
inverse
relation
between
maternal
education
and
improved
birth
outcomes
is
evident.
Women
with
less
than
a
high
school
education
show
significant
improvements
in
birthweight,
LBW
status,
and
adequacy
of
prenatal
care.
Stratification
of
the
sample
by
birth
parity
revealed
no
consistent
pattern.
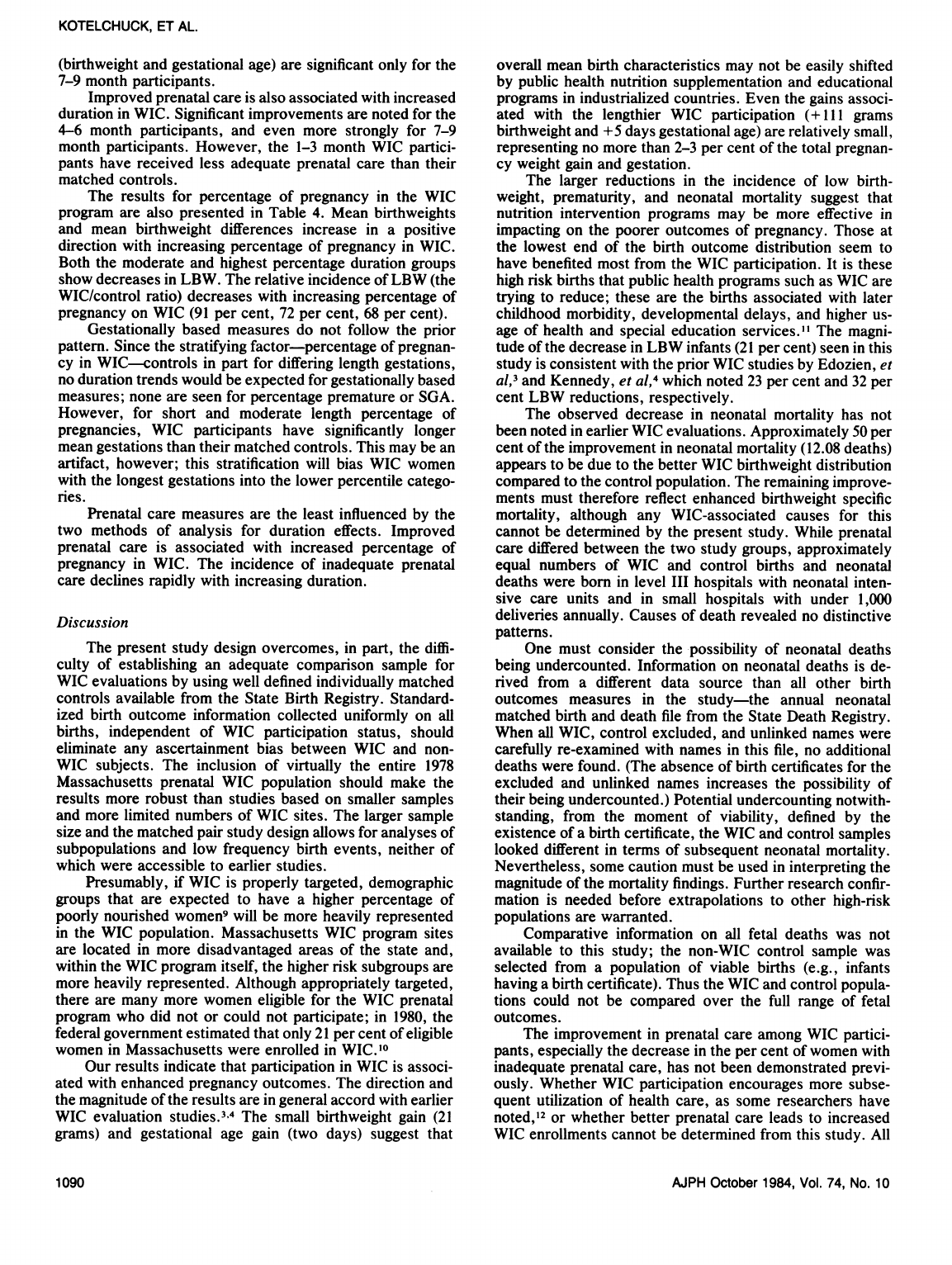
Increased
Duration
of
WIC
Participation-Duration
of
prenatal
participation
in
WIC
is
based
on
the
number
of
months
between
the
month
of
the
first
redemption
of
a
voucher
and
the
month
of
delivery.
The
mean
duration
of
prenatal
participation
in
WIC
in
1978
was
4.6
months.
The
cumulative
impact
of
WIC
participation
on
birth
outcomes
was
examined
in
two
ways.
First,
WIC
partici-
pants
and
their
matched
controls
were
stratified
into
three
groups
based
on
absolute
number
of
months
in
the
WIC
program:
33
per
cent
participated
for
one
to
three
months;
45
per
cent
for
four
to
six
months;
and
22
per
cent
for
seven
to
nine
months.
Second,
to
compensate
partially
for
differing
lengths
of
gestation,
participants
were
also
stratified
into
four
groups
based
on
percentage
of
pregnancy
in
the
WIC
AJPH
October
1984,
Vol.
74,
No.
10
1088
WIC
PARTICIPATION,
PREGNANCY
OUTCOME:
MASSACHUSETTS
TABLE
3-Selcted
Birth
Outcome
Dier
by
Dmographic
Subpopuations
(WIC
Minus
Control)
Birthweight
LBW
Gestation
Inadequate
Subpopulation
N
Difference
Difference
Difference
Care
Difference
Matemal
Age
(years)
s15
95
98
-3.2
.5
-11.6
s17
504 57
-3.20
.5*
-7.3***
519
1178
380
-3.0*
.4***
-5.2***
20-34
2781
16
-3.2°
.1
-2.3***
34+
162
-10
-4.9
.2
-0.6
Race/Ethnicity
Hispanic
origin
906
65*
-2.4*
.3'
0.8
Black
978
37
-2.1
.3
-4.6***
White
3010
14
-1.7"
.2***
-2.6***
White-Hispanic
2298
8
-1.3
.2**
-2.7'
Marital
Status
Unmarried
1677
350
-2.5*"
.3***
-6.r**
Married
2445
14
-1.2
.1
-0.5
Education
(years)
<12
2033
36*
-2.5
.2
-4.4***
12
1498
2
-1.4
.3*"
-4.0**"
>12
468
10
-1.0
.1
-1.3
Parity
1
1852
14
-1.6'
.3**
-4.0"**
2-3
1956
12
-1.6
.2
-1.5*
4+
520
20
-3.3'
.1
-4.8*
o
p
<
.10.
p
<
.05.
=p
<.01.
'=p
<.0o1.
program:
32
per
cent
participated
for
0-40
per
cent
of
their
pregnancy;
40
per
cent
participated
for
41-70
per
cent;
20
per
cent
participated
for
71-100
per
cent;
and
8
per
cent
had
unknown
gestations.
The
results
for
duration
in
the
WIC
prenatal
program
by
number
of
months
are
presented
in
Table
4.
Increased
duration
in
WIC
is
associated
with
enhanced
pregnancy
outcomes.
In
particular,
increased
duration
is
significantly
associated
with
increases
in
mean
birthweight
and
gestation-
al
age,
and
decreases
in
the
incidence
of
low
birthweight,
prematurity,
small
for
gestational
age
(SGA),
and
neonatal
deaths.
The
findings
are
strongest
for
the
7-9
month
partici-
pants.
It
would
appear
that
the
reduction
in
the
incidence
of
some
of
the
poorer
marginal
pregnancy
outcomes
(LBW
and
neonatal
mortality)
is
significant
from
4-6
months
of
partici-
pation,
while
enhancement
of
mean
birth
characteristics
TABLE
4-Selcted
Birth
Outcome
Meurse
by
Duration
WIC
Participation
Months
WIC
Participation
Per
Cent
of
Pregnancy
WIC
Participation
Birth
Outcome
1-3
4-6
7-9
Unknown
0-40%
41-70%
71-100%O
Birthweight
(grams)
WiC
3236
3264
3385"'
3272
3260
3269
3341'
Control
3260 3253
3274
3245
3254
3252
3291
Low
Brithweight
%
WIC
8.2
7.6'
3.4"*'
7.7
8.0
7.6*
5.9'
Control
7.8 9.5 8.6
10.8
8.7
10.5
8.6
Gestational
Age
(weeks)
WiC
39.8
39.8
40.4*"*
39.8
40.1"
39.9"*
39.8
Control
39.8
39.8
39.7
39.9
39.8
39.7
39.8
Premature
(<37
weeks)
WiC
10.7
9.1
4.3"*'
12.9
10.5
8.5
9.5
Control
9.5
9.4
9.5
9.7
11.5
11.2
9.7
Small
for
Gestational
Age
%
WiC
5.3
5.2
2.6*
8.2
6.2
6.4
4.8
Control
4.5
5.4
4.7
6.5
5.2
5.9
5.2
Neonatal
Mortality
(#)
WIC
7
5*
0*
1
4
5
2
Control
12
15
8
4
13
11
7
Inadequate
Prenatal
Care
%
WIC
7.7
2.6"**
0.6*"'
8.8
7.4
2.7"**
0.6***
Control
6.8
7.7
5.6
8.6
6.8
8.7
5.8
Total
(N)
(1365) (1848)
(909)
(308)
(1307)
(1664)
(844)
p
<
.10.
p
<
.05.
=
p
<
.01.
=p
<
.001.
AJPH
October
1984,
Vol.
74,
No.
10
1089
KOTELCHUCK,
ET
AL.
(birthweight
and
gestational
age)
are
significant
only
for
the
7-9
month
participants.
Improved
prenatal
care
is
also
associated
with
increased
duration
in
WIC.
Significant
improvements
are
noted
for
the
4-6
month
participants,
and
even
more
strongly
for
7-9
month
participants.
However,
the
1-3
month
WIC
partici-
pants
have
received
less
adequate
prenatal
care
than
their
matched
controls.
The
results
for
percentage
of
pregnancy
in
the
WIC
program
are
also
presented
in
Table
4.
Mean
birthweights
and
mean
birthweight
differences
increase
in
a
positive
direction
with
increasing
percentage
of
pregnancy
in
WIC.
Both
the
moderate
and
highest
percentage
duration
groups
show
decreases
in
LBW.
The
relative
incidence
of
LBW
(the
WIC/control
ratio)
decreases
with
increasing
percentage
of
pregnancy
on
WIC
(91
per
cent,
72
per
cent,
68
per
cent).
Gestationally
based
measures
do
not
follow
the
prior
pattern.
Since
the
stratifying
factor-percentage
of
pregnan-
cy
in
WIC-controls
in
part
for
differing
length
gestations,
no
duration
trends
would
be
expected
for
gestationally
based
measures;
none
are
seen
for
percentage
premature
or
SGA.
However,
for
short
and
moderate
length
percentage
of
pregnancies,
WIC
participants
have
significantly
longer
mean
gestations
than
their
matched
controls.
This
may
be
an
artifact,
however;
this
stratification
will
bias
WIC
women
with
the
longest
gestations
into
the
lower
percentile
catego-
ries.
Prenatal
care
measures
are
the
least
influenced
by
the
two
methods
of
analysis
for
duration
effects.
Improved
prenatal
care
is
associated
with
increased
percentage
of
pregnancy
in
WIC.
The
incidence
of
inadequate
prenatal
care
declines
rapidly
with
increasing
duration.
Discussion
The
present
study
design
overcomes,
in
part,
the
diffi-
culty
of
establishing
an
adequate
comparison
sample
for
WIC
evaluations
by
using
well
defined
individually
matched
controls
available
from
the
State
Birth
Registry.
Standard-
ized
birth
outcome
information
collected
uniformly
on
all
births,
independent
of
WIC
participation
status,
should
eliminate
any
ascertainment
bias
between
WIC
and
non-
WIC
subjects.
The
inclusion
of
virtually
the
entire
1978
Massachusetts
prenatal
WIC
population
should
make
the
results
more
robust
than
studies
based
on
smaller
samples
and
more
limited
numbers
of
WIC
sites.
The
larger
sample
size
and
the
matched
pair
study
design
allows
for
analyses
of
subpopulations
and
low
frequency
birth
events,
neither
of
which
were
accessible
to
earlier
studies.
Presumably,
if
WIC
is
properly
targeted,
demographic
groups
that
are
expected
to
have
a
higher
percentage
of
poorly
nourished
women9
will
be
more
heavily
represented
in
the
WIC
population.
Massachusetts
WIC
program
sites
are
located
in
more
disadvantaged
areas
of
the
state
and,
within
the
WIC
program
itself,
the
higher
risk
subgroups
are
more
heavily
represented.
Although
appropriately
targeted,
there
are
many
more
women
eligible
for
the
WIC
prenatal
program
who
did
not
or
could
not
participate;
in
1980,
the
federal
government
estimated
that
only
21
per
cent
of
eligible
women
in
Massachusetts
were
enrolled
in
WIC.10
Our
results
indicate
that
participation
in
WIC
is
associ-
ated
with
enhanced
pregnancy
outcomes.
The
direction
and
the
magnitude
of
the
results
are
in
general
accord
with
earlier
WIC
evaluation
studies.34
The
small
birthweight
gain
(21
grams)
and
gestational
age
gain
(two
days)
suggest
that
overall
mean
birth
characteristics
may
not
be
easily
shifted
by
public
health
nutrition
supplementation
and
educational
programs
in
industrialized
countries.
Even
the
gains
associ-
ated
with
the
lengthier
WIC
participation
(+
111
grams
birthweight
and
+5
days
gestational
age)
are
relatively
small,
representing
no
more
than
2-3
per
cent
of
the
total
pregnan-
cy
weight
gain
and
gestation.
The
larger
reductions
in
the
incidence
of
low
birth-
weight,
prematurity,
and
neonatal
mortality
suggest
that
nutrition
intervention
programs
may
be
more
effective
in
impacting
on
the
poorer
outcomes
of
pregnancy.
Those
at
the
lowest
end
of
the
birth
outcome
distribution
seem
to
have
benefited
most
from
the
WIC
participation.
It
is
these
high
risk
births
that
public
health
programs
such
as
WIC
are
trying
to
reduce;
these
are
the
births
associated
with
later
childhood
morbidity,
developmental
delays,
and
higher
us-
age
of
health
and
special
education
services."
The
magni-
tude
of
the
decrease
in
LBW
infants
(21
per
cent)
seen
in
this
study
is
consistent
with
the
prior
WIC
studies
by
Edozien,
et
al,3
and
Kennedy,
et
al,4
which
noted
23
per
cent
and
32
per
cent
LBW
reductions,
respectively.
The
observed
decrease
in
neonatal
mortality
has
not
been
noted
in
earlier
WIC
evaluations.
Approximately
50
per
cent
of
the
improvement
in
neonatal
mortality
(12.08
deaths)
appears
to
be
due
to
the
better
WIC
birthweight
distribution
compared
to
the
control
population.
The
remaining
improve-
ments
must
therefore
reflect
enhanced
birthweight
specific
mortality,
although
any
WIC-associated
causes
for
this
cannot
be
determined
by
the
present
study.
While
prenatal
care
differed
between
the
two
study
groups,
approximately
equal
numbers
of
WIC
and
control
births
and
neonatal
deaths
were
born
in
level
III
hospitals
with
neonatal
inten-
sive
care
units
and
in
small
hospitals
with
under
1,000
deliveries
annually.
Causes
of
death
revealed
no
distinctive
patterns.
One
must
consider
the
possibility
of
neonatal
deaths
being
undercounted.
Information
on
neonatal
deaths
is
de-
rived
from
a
different
data
source
than
all
other
birth
outcomes
measures
in
the
study-the
annual
neonatal
matched
birth
and
death
file
from
the
State
Death
Registry.
When
all
WIC,
control
excluded,
and
unlinked
names
were
carefully
re-examined
with
names
in
this
file,
no
additional
deaths
were
found.
(The
absence
of
birth
certificates
for
the
excluded
and
unlinked
names
increases
the
possibility
of
their
being
undercounted.)
Potential
undercounting
notwith-
standing,
from
the
moment
of
viability,
defined
by
the
existence
of
a
birth
certificate,
the
WIC
and
control
samples
looked
different
in
terms
of
subsequent
neonatal
mortality.
Nevertheless,
some
caution
must
be
used
in
interpreting
the
magnitude
of
the
mortality
findings.
Further
research
confir-
mation
is
needed
before
extrapolations
to
other
high-risk
populations
are
warranted.
Comparative
information
on
all
fetal
deaths
was
not
available
to
this
study;
the
non-WIC
control
sample
was
selected
from
a
population
of
viable
births
(e.g.,
infants
having
a
birth
certificate).
Thus
the
WIC
and
control
popula-
tions
could
not
be
compared
over
the
full
range
of
fetal
outcomes.
The
improvement
in
prenatal
care
among
WIC
partici-
pants,
especially
the
decrease
in
the
per
cent
of
women
with
inadequate
prenatal
care,
has
not
been
demonstrated
previ-
ously.
Whether
WIC
participation
encourages
more
subse-
quent
utilization
of
health
care,
as
some
researchers
have
noted,'2
or
whether
better
prenatal
care
leads
to
increased
WIC
enrollments
cannot
be
determined
from
this
study.
All
AJPH
October
1984,
Vol.
74,
No.
10
1090

WIC
PARTICIPATION,
PREGNANCY
OUTCOME:
MASSACHUSETTS
prenatal
WIC
participants
must
document
their
pregnancy
status,
an
act
that
encourages
a
formal
prenatal
care
visit
and
thereby
increases
the
likelihood
of
being
drawn
at
an
early
stage
into
a
prenatal
care
health
network.
Improved
prenatal
care
is
both
an
important
goal
and
an
achievement
of
the
WIC
program.
Benefits
associated
with
WIC
participation
do
not
ap-
pear
limited
to
any
particular
population
group,
but
are
seen
across
a
wide
spectrum
of
subpopulations.
Subpopulations
at
higher
nutritional
risk
for
poor
pregnancy
outcomes,
however,
appear
to
benefit
more
strongly,
especially
teen-
age,
unmarried,
and
Hispanic
origin
women.
In
general,
the
neediest
populations
seem
to
benefit
the
most
from
the
WIC
program.
Increased
duration
of
participation
in
the
WIC
program
appears
to
be
associated
with
enhanced
birth
outcomes,
in
general
accord
with
prior
WIC
research.3'4
The
birth
out-
comes
for
the
longest
duration
WIC
participants
reach
or
surpass
the
State's
overall
mean
birthweight
(3343
grams)
and
incidence
of
LBW
(6.55
per
cent).
Estimating
the
exact
magnitude
of
the
cumulative
bene-
fits
associated
with
increased
duration
of
participation
in
WIC
is
methodologically
complicated.
Duration
of
participa-
tion
and
gestational
age
are,
in
part,
confounded.
WIC
benefits
may
be
mediated
through
increased
gestational
age
but
in
turn,
increased
gestational
age
allows
for
increased
duration
in
WIC.
Any
grouping
of
subjects
for
statistical
analysis
on
the
basis
of
extensive
absolute
duration
of
participation
in
WIC
virtually
assures
that
they
have
longer
gestations
and
higher
birthweight;
while
any
statistical
cor-
rections
for
length
of
gestation
will
eliminate
the
benefits
associated
with
the
program's
enhancement
of
gestational
age.
Since
no
ideal
analytic
solution
exists,'3
we
used
two
alternative
methods:
absolute
duration
in
WIC,
and
percent-
age
of
pregnancy
in
WIC.
Since
the
absolute
duration
measure
may
be
an
over-estimation
and
the
percentage
of
pregnancy
may
be
an
under-estimation,
we
suggest
that
the
magnitude
of
the
cumulative
benefits
associated
with
WIC
should
fall
between
these
two
estimates.
Both
methods
of
analyses
imply
that
more
extensive
WIC
participation
is
associated
with
more
beneficial
birth
outcomes.
The
abso-
lute
duration
analysis
would
indicate
that
the
benefits
are
not
simply
linear;
WIC
participation
greater
than
six
months
would
appear
maximally
beneficial.
It
is
not
only
chance
or
self-motivation
that
determines
if
a
person
enters
WIC
early
or
late.
Barriers
and
incentives
to
early
participation
exist.
Haddad
and
Willis'4
have
shown
that
the
probability
of
women
entering
WIC
in
their
first
three
months
of
pregnancy
is
significantly
enhanced
if
the
WIC
program
site
has
been
open
a
long
time,
delivers
it
supplementation
through
retail
stores,
and
uses
public
ser-
vice
announcements.
The
potential
benefits
associated
with
the
WIC
program
are
not
yet
being
reached;
only
22
per
cent
of
the
WIC
prenatal
participants
participated
for
more
than
six
months.
The
comprehensiveness
of
the
case
population
is
an
important
element
in
assessing
the
validity
and
generalizabi-
lity
of
the
present
study.
The
names
of
525
women
adminis-
tratively
excluded
from
the
WIC
prenatal
program
were
omitted
from
this
study.
Unfortunately,
very
little
demo-
graphic
or
motivational
information
is
available
about
them
from
the
WIC
computerized
records.
The
353
names,
which
had
no
reason
specified
for
their
exclusion,
were
similar
racially
to
the
WIC
study
population
(68.6
per
cent
White
excluded
group
vs
73.6
per
cent
study
group).
We
are
doubtful
that
most
of
these
353
names
led
to
an
actual
Massachusetts
birth.
Less
than
10
per
cent
of
these
women
had
locatable
birth
certificates.
Abortions,
fraud,
computer
errors,
and
out-of-state
moves
are
the
more
likely
unrecord-
ed
realities
for
these
names.t
Women
do
not
always
inform
the
WIC
program
of
their
reasons
for
discontinuance.
Nev-
ertheless,
one
cannot
rule
out
of
the
possibility
that
the
administratively
excluded
names
may
have
had
specific
characteristics
which
would
bias
the
overall
study
results.
The
birth
certificates
for
191
women
who
were
in
the
WIC
program
prenatally
could
not
be
located.
Again,
little
epidemiologic
information
is
available
about
these
women.
Racially
(based
on
their
WIC
records)
they
are
similar;
their
duration
of
participation
in
WIC
is
essentially
the
same
as
the
WIC
group.
No
fetal
deaths
were
located
among
this
group.
One
can
not
rule
out
the
possibility
that
they
may
have
had
specific
characteristics
which
would
bias
the
overall
results.
Five
WIC
women
with
birth
certificates
were
not
matched
to
controls.
Overall,
we
estimate
that
at
least
95
per
cent
of
the
WIC
prenatal
participant
population
were
included
in
the
study
which
represents
the
largest
and
most
comprehensive
series
on
WIC
prenatal
participants
to
date.
Establishing
the
existence
and
magnitude
of
a
WIC
program
effect
also
depends
critically
on
the
comparability
of
the
WIC
and
matched
control
groups.
Unfortunately,
there
are
inherent
limitations
to
the
conclusions
that
can
be
drawn
from
a
retrospective
cohort
study
in
which
the
exposure
(WIC)
group
is
self-selected
and
the
control
group
is
derived
by
a
post-hoc
matching
procedure.
A
more
ideal
randomized
case
control
study
would
pose
serious
ethical
dilemmas.
Since
many
known
confounding
factors
have
been
controlled,
we
believe
that
the
statistical
differences
between
the
WIC
and
control
groups
are
a
function
of
WIC
participation;
however,
additional
confounding
factors
may
also
be
characteristic
of
the
WIC
or
control
populations
and
account
for
any
birth
outcome
differences
noted.
The
Massachusetts
birth
certificates
do
not
provide
specific
information
on
maternal
pre-pregnancy
weight
or
height,
maternal
weight
gain,
maternal
smoking
habits,
or
maternal
morbidity.
Any
of
these
factors,
if
unevenly
distrib-
uted,
may
be
sufficient
to
distort
the
overall
outcomes.
WIC
participants
may
be
more
strongly
motivated
to
improve
the
prenatal
health
of
their
future
offspring
than
are
the
control
women.
Such
a
motivational
difference
could
cause
both
an
improvement
in
pregnancy
outcome
and
a
desire
to
enroll
in
the
WIC
program.
The
findings
of
earlier
and
more
frequent
prenatal
care
visits
may
be
supportive
of
this
view.
The
increase
in
prenatal
care
may
also
be
the
cause
of
the
improved
birth
outcomes,
and
not
simply
another
conse-
quence
of
WIC
participation.
The
lack
of
prenatal
care
improvements
among
Hispanic
origin
women
who
show
enhanced
birth
outcomes
argues
somewhat
against
this
interpretation.
The
present
study
design
does
not
lend
itself
to
a
study
of
prenatal
care,
nutrition
supplementation,
or
nutrition
counseling
independently
of
each
other.
Although
these
alternative
explanations
for
the
birth
outcome
differences
tend
to
suggest
that
the
attributed
WIC
program
effects
may
be
over-estimated,
an
under-estimation
may
be
just
as
likely.
The
WIC
population
could
be
financial-
t
Women
who
delivered
prematurely,
even
shortly
after
joining
the
WIC
program,
would
not
be
administratively
excluded;
these
women
would
be
switched
to
the
WIC
postpartum
program
and
their birth
records
included
in
this
study.
AJPH
October
1984,
Vol.
74,
No.
10
1091
KOTELCHUCK,
ET
AL.
ly
poorer
and
at
greater
obstetric
risk
than
their
matched
controls.
All
WIC
participants
must
have
an
income
under
195
per
cent
of
the
poverty
level,
while
the
controls
have
no
restrictions
on
income,
and
presumably
some
have
higher
incomes.
Post-hoc
analyses
reveal
that
there
were
more
women
of
Hispanic
origin
in
the
WIC
than
the
control
sample
(906
vs
509).
And
WIC
participants
are
selected,
in
part,
on
the
basis
of
poor
prior
obstetrical
histories,
while
no
such
criteria
exists
for
the
control
group.
These
potential
confounding
factors
in
a
matched
study
design
would
de-
crease
the
likelihood
of
showing
positive
birth
outcomes
associated
with
WIC
participation.
In
summary,
the
Massachusetts
WIC
Statewide
Evalua-
tion
Project
compared
the
birth
outcomes
of
4,126
WIC
prenatal
participants
and
4,126
individually
matched
con-
trols,
utilizing
public
birth
and
death
certificates.
Results
showed
that
the
WIC
program
appears
to
be
targeted
to
women
at
high
demographic
risk
for
poor
pregnancy
out-
comes;
that
overall
WIC
participation
is
associated
with
small
improvements
in
mean
birth
characteristics,
larger
reductions
in
marginal
pregnancy
outcomes,
and
enhanced
prenatal
care;
and,
that
these
benefits
are
observed
more
strongly
in
higher
risk
subpopulations
and
are
enhanced
with
increased
duration
of
participation.
Based
on
the
informa-
tion
available
to
this
study,
we
conclude
that
participation
in
the
WIC
prenatal
program
is
associated
with
improved
pregnancy
outcomes
for
women
at
high
nutritional
and
financial
risk.
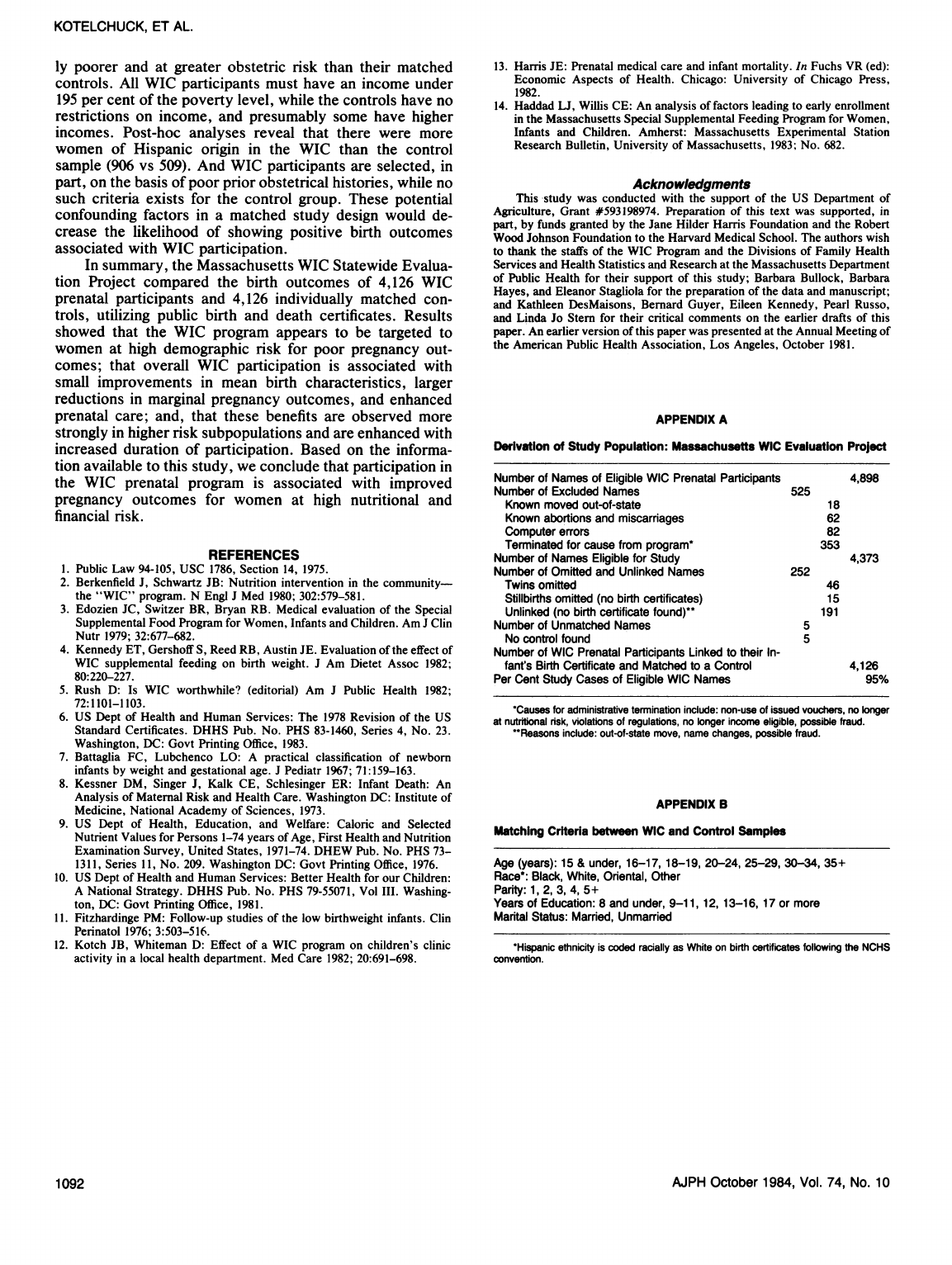
REFERENCES
1.
Public
Law
94-105,
USC
1786,
Section
14,
1975.
2.
Berkenfield
J,
Schwartz
JB:
Nutrition
intervention
in
the
community-
the
"WIC"
program.
N
Engi
J
Med
1980;
302:579-581.
3.
Edozien
JC,
Switzer
BR,
Bryan
RB.
Medical
evaluation
of
the
Special
Supplemental
Food
Program
for
Women,
Infants
and
Children.
Am
J
Clin
Nutr
1979;
32:677-682.
4.
Kennedy
ET,
Gershoff
S,
Reed
RB,
Austin
JE.
Evaluation
of
the
effect
of
WIC
supplemental
feeding
on
birth
weight.
J
Am
Dietet
Assoc
1982;
80:220-227.
5.
Rush
D:
Is
WIC
worthwhile?
(editorial)
Am
J
Public
Health
1982;
72:1101-1103.
6.
US
Dept
of
Health
and
Human
Services:
The
1978
Revision
of
the
US
Standard
Certificates.
DHHS
Pub.
No.
PHS
83-1460,
Series
4,
No.
23.
Washington,
DC:
Govt
Printing
Office,
1983.
7.
Battaglia
FC,
Lubchenco
LO:
A
practical
classification
of
newborn
infants
by
weight
and
gestational
age.
J
Pediatr
1967;
71:159-163.
8.
Kessner
DM,
Singer
J,
Kalk
CE,
Schlesinger
ER:
Infant
Death:
An
Analysis
of
Maternal
Risk
and
Health
Care.
Washington
DC:
Institute
of
Medicine,
National
Academy
of
Sciences,
1973.
9.
US
Dept
of
Health,
Education,
and
Welfare:
Caloric
and
Selected
Nutrient
Values
for
Persons
1-74
years
of
Age,
First
Health
and
Nutrition
Examination
Survey,
United
States,
1971-74.
DHEW
Pub.
No.
PHS
73-
1311,
Series
11,
No.
209.
Washington
DC:
Govt
Printing
Office,
1976.
10.
US
Dept
of
Health
and
Human
Services:
Better
Health
for
our
Children:
A
National
Strategy.
DHHS
Pub.
No.
PHS
79-55071,
Vol
III.
Washing-
ton,
DC:
Govt
Printing
Office,
1981.
11.
Fitzhardinge
PM:
Follow-up
studies
of
the
low
birthweight
infants.
Clin
Perinatol
1976;
3:503-516.
12.
Kotch
JB,
Whiteman
D:
Effect
of
a
WIC
program
on
children's
clinic
activity
in
a
local
health
department.
Med
Care
1982;
20:691-698.
13.
Harris
JE:
Prenatal
medical
care
and
infant
mortality.
In
Fuchs
VR
(ed):
Economic
Aspects
of
Health.
Chicago:
University
of
Chicago
Press,
1982.
14.
Haddad
LJ,
Willis
CE:
An
analysis
of
factors
leading
to
early
enrollment
in
the
Massachusetts
Special
Supplemental
Feeding
Program
for
Women,
Infants
and
Children.
Amherst:
Massachusetts
Experimental
Station
Research
Bulletin,
University
of
Massachusetts,
1983;
No.
682.
Acknowledgments
This study
was
conducted
with
the
support
of
the
US
Department
of
Agriculture,
Grant
#593198974.
Preparation
of
this
text
was
supported,
in
part,
by
funds
granted
by
the
Jane
Hilder
Harris
Foundation
and
the
Robert
Wood
Johnson
Foundation
to
the
Harvard
Medical
School.
The
authors
wish
to
thank
the
staffs
of
the
WIC
Program
and
the
Divisions
of
Family
Health
Services
and
Health
Statistics
and
Research
at
the
Massachusetts
Department
of
Public
Health
for
their
support
of
this
study;
Barbara
Bullock,
Barbara
Hayes,
and
Eleanor
Stagliola
for
the
preparation
of
the
data
and
manuscript;
and
Kathleen
DesMaisons,
Bernard
Guyer,
Eileen
Kennedy,
Pearl
Russo,
and
Linda
Jo
Stern
for
their
critical
comments
on
the
earlier
drafts
of
this
paper.
An
earlier
version
of
this
paper
was
presented
at
the
Annual
Meeting
of
the
American
Public
Health
Association,
Los
Angeles,
October
1981.
APPENDIX
A
Derivation
of
Study
Population:
Massachusetts
WIC
Evaluation
Project
Number
of
Names
of
Eligible
WIC
Prenatal
Participants
4,898
Number
of
Excluded
Names
525
Known
moved
out-of-state
18
Known
abortions
and
miscarriages
62
Computer
errors
82
Terminated
for
cause
from
program*
353
Number
of
Names
Eligible
for
Study
4,373
Number
of
Omitted
and
Unlinked
Names
252
Twins
omitted
46
Stillbirths
omitted
(no
birth
certificates)
15
Unlinked
(no
birth
certificate
found)**
191
Number
of
Unmatched
Names
5
No
control
found
5
Number
of
WIC
Prenatal
Participants
Linked
to
their
In-
fant's
Birth
Certificate
and
Matched
to
a
Control
4,126
Per
Cent
Study
Cases
of
Eligible
WIC
Names
95%
*Causes
for
administrative
termination
include:
non-use
of
issued
vouchers,
no
longer
at
nutritional
risk,
violations
of
regulations,
no
longer
income
eligible,
possible
fraud.
"Reasons
include:
out-of-state
move,
name
changes,
possible
fraud.
APPENDIX
B
Matching
Criteria
between
WIC
and
Control
Samples
Age
(years):
15
&
under,
16-17, 18-19,
20-24,
25-29,
30-34,
35+
Race*:
Black,
White,
Oriental,
Other
Parity:
1,
2,
3,
4,
5+
Years
of
Education:
8
and
under,
9-11,
12,
13-16,
17
or
more
Marital
Status:
Married,
Unmarried
*Hispanic
ethnicity
is
coded
racially
as
White
on
birth
certificates
following
the
NCHS
convention.
1092
AJPH
October
1984,
Vol.
74,
No.
10
