
1
2
3
4
Calling
Your Health
Plan
page 7
Fact
Sheet
pages 2-3
Types of
Coverage
page 4
EXPANDING THE POSSIBILITIES
toolkit
New Benets for Breastfeeding Moms:
Facts and Tools to Understand Your Coverage
under the Health Care Law
5
6
Sample
Appeal
Letters
pages 9-11
Sample
Script
page 8
Questions
& Answers
pages 5-6

© 2014 National Women’s Law Center
ABOUT THE CENTER
The National Women’s Law Center is
a non-prot organization that has been
working since 1972 to advance and
protect women’s equality and opportunity.
The Center focuses on major policy
areas of importance to women and their
families, including economic security,
education, employment and health,
with special attention given to the
concerns of low-income women.
For more information about the Center
or to make a tax-deductible contribution
to support the Center’s work, please visit:
www.nwlc.org or call the Development
ofce at 202-588-5180.
AUTHORS
This Toolkit was a collaborative
endeavor that relied upon the work
of many individuals. The primary
authors—Anna Benyo and Stephanie
Glover—were greatly assisted by
Marcia Greenberger, Judy Waxman,
and Karen Davenport. Beth Stover
designed the Toolkit with layout/design
assistance provided by Nancy Magill.
DISCLAIMER
While text and citations are, to the
best of the authors’ knowledge, current
as this report was prepared, there may
well be subsequent developments,
including new administrative guidance,
that could alter the information provided
herein. This report does not constitute
legal advice; individuals and organizations
considering legal action should consult
with their own legal counsel before
deciding on a course of action. In addition,
this report does not constitute medical
advice. Individuals with health problems
should consult an appropriate health
care provider.
NATIONAL WOMEN’S LAW CENTER
NWLC NEW BENEFITS FOR BREASTFEEDING MOMS 1
The health care law requires new health plans to cover certain preventive services without any cost-sharing. This
means that, as Americans enroll in new coverage options made possible by the Affordable Care Act (ACA), and an
increasing number of existing health plans come under the law’s reach, more and more people will have access to a
wide range of preventive services without co-payments, deductibles, or co-insurance. This is especially important to
women, who are more likely than men to avoid needed health care, including preventive care, because of cost.
As part of women’s preventive services, new plans are required to cover breastfeeding support, supplies, and
counseling. This is a signicant step forward in making breastfeeding more accessible and affordable for millions of
Americans.
This toolkit is designed for women, advocates, community-based organizations and health care providers to provide
information on the coverage of breastfeeding support, supplies, and counseling in the health care law and offer tools
to women who encounter problems with this coverage. We have also provided detailed instructions on how to call
insurance companies and how to le an appeal if the plan denies coverage. The toolkit includes draft appeal letters
tailored to commonly encountered scenarios.
If you have any questions or need further guidance, contact the National Women’s Law Center at 1-866-745-5487
or [email protected]. We are interested in hearing from you. Please let us know if you use this toolkit to obtain
coverage successfully.
Introduction

NATIONAL WOMEN’S LAW CENTER
2 NEW BENEFITS FOR BREASTFEEDING MOMS NWLC
The Affordable Care Act (ACA) makes breastfeeding more accessible and affordable for millions of American women.
The law requires that all new health plans must provide certain preventive services without any cost-sharing, including
coverage for breastfeeding support and supplies. Breastfeeding benets the mother and the child, but too often there
is a gap between women’s desire to breastfeed their babies and the support they need to successfully breastfeed.
Although a majority of women plan to breastfeed, a much lower proportion actually do when they are discharged from
the hospital after delivery.
1
In order to support women’s efforts to breastfeed, and reduce cost as a barrier, the health
care law requires new plans to cover breastfeeding supplies, and support and counseling without co-payments,
deductibles, or co-insurance.
HEALTH INSURANCE PLANS MUST COVER WOMEN’S PREVENTIVE SERVICES
The health care law requires most insurance plans to offer a range of preventive services and took special steps to
ensure coverage of new preventive services that are important to women. These services were developed by the
Institute of Medicine and endorsed by the Health Resources Services Administration (HRSA). They include: (1)
Breastfeeding support, supplies, and counseling; (2) Screening and counseling for interpersonal and domestic
violence; (3) Screening for gestational diabetes; (4) DNA testing for high-risk strains of HPV; (5) Counseling regarding
sexually transmitted infections, including HIV; (6) Screening for HIV; (7) Contraceptive methods and counseling; and
(8) Well woman visits.
BREASTFEEDING EQUIPMENT AND SUPPLIES
All new health plans must cover breastfeeding equipment and supplies “for the duration of breastfeeding” without
cost-sharing, which means plans may not apply any co-payment, co-insurance, or deductible to these benets.
Breastfeeding equipment and supplies most commonly refers to a breast pump, which is a device that extracts milk
from a lactating woman, and related accessories. The FDA, which regulates breast pumps, states that they can be
“used to maintain or increase a woman’s milk supply, relieve engorged breasts and plugged milk ducts, or pull out
at or inverted nipples so a nursing baby can latch-on to its mother’s breast more easily.”
2
Many women use breast
pumps to express and store their milk after they have returned to work, are traveling, or have to be away from their
breastfeeding child. (Also, employers are required to provide a clean, private place for women to pump while on the
job.)
While a health insurer must cover breastfeeding equipment and supplies, it can impose some requirements on this
coverage, such as requiring a purchase, rather than rental, of a breast pump.
COMPREHENSIVE LACTATION SUPPORT AND COUNSELING
The health care law requires all new health plans to cover “comprehensive prenatal and postnatal lactation support
[and] counseling.” This means that breastfeeding mothers have health insurance coverage for lactation counseling
without cost-sharing for as long as they are breastfeeding. Lactation consultants are trained specialists who work
with women to help them begin and continue to breastfeed. Health insurers must cover such consultations without
cost-sharing, but can require consumers to see only the providers on their list, called “in-network providers,” or impose
other requirements on coverage.
Factsheet:
New Benets for Breastfeeding Moms
1 Institute of Medicine, “Clinical Preventive Services for Women: Closing the Gaps,” (2011), the National Academies Press.
2 U.S. Food and Drug Administration, “Breast Pumps,” available at http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/
HomeHealthandConsumer/ConsumerProducts/BreastPumps/default.htm.

NATIONAL WOMEN’S LAW CENTER
NWLC NEW BENEFITS FOR BREASTFEEDING MOMS 3
DIFFERENCES IN COVERAGE
The requirement to cover breastfeeding support and supplies applies to all new plans. Because some health plans
existed before the health care law was passed, some differences in coverage still remain (also see the ow chart
entitled “Does my insurance plan have to cover breastfeeding supplies and support without cost sharing?”).
Medicaid and Medicaid Expansion
The requirement to provide breastfeeding support and supplies will vary by state and by type of Medicaid coverage.
Traditional Medicaid programs already cover a wide range of preventive services for Medicaid enrollees with nominal
or no co-payments. They are not, however, required to provide this new benet under the ACA. This means that
traditional Medicaid programs, including pregnancy-related coverage, are not required to provide breastfeeding support
and supplies but many states choose to provide these benets. Based on a 2012 survey with 44 states responding,
25 states covered breastfeeding education services, 15 states covered individual lactation consultations, and 31 states
covered equipment rentals.
3
The ACA allows states to expand eligibility for Medicaid to cover more low income people up to 138 percent of the
federal poverty level (approximately $16,000 for an individual or $33,000 for a family of four). However, each state
decides whether or not to expand eligibility. About half the states have expanded coverage through Medicaid. States
that have expanded coverage are required to provide coverage of breastfeeding support and supplies for individuals
newly eligible for Medicaid under this expansion.
In short, depending on where they live, traditional Medicaid enrollees may not have coverage for breastfeeding support
and supplies. However, Medicaid enrollees who are newly eligible and covered as part of the “Medicaid expansion” will
have coverage for these services.
Employer Sponsored Coverage
Most employees and their dependents who have health insurance through an employer are enrolled in plans that
must provide coverage for breastfeeding support and supplies. Plans that existed before March 23, 2010, and have
not made signicant changes, are considered “grandfathered,” and do not need to cover preventive services, includ-
ing breastfeeding benets. If the plan makes signicant changes (like increasing employee costs or cutting benets), it
will become “ungrandfathered.” All un-grandfathered private health plans have to follow the preventive health services
coverage and offer breastfeeding support and supplies at no cost-sharing.
In 2013, only 36 percent of workers with employer sponsored coverage were in grandfathered plans, and more plans
will become ungrandfathered in 2014.
4
Eventually all plans will lose their grandfathered status and distinctions between
the two types of plans will disappear. At that point, all plans will cover these important preventive services without
cost-sharing.
Individual Coverage
All plans purchased on the Health Insurance Marketplaces are considered “new” plans and are required to cover
breastfeeding support and supplies.
Individual plans purchased outside of the Marketplace generally have to provide coverage of breastfeeding benets
as well. However, there is a small portion of individually purchased private plans that are not required to provide this
coverage. If an individual has been enrolled in the same plan since before March 23, 2010, then the plan is considered
“grandfathered,” meaning that it doesn’t have to comply with the health care law.
3 Centers for Medicare and Medicare Services, “Medicaid Coverage of Lactation Services,” (January 10, 2012) available at
http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Quality-of-Care/Downloads/Lactation_Services_IssueBrief_01102012.
pdf.
4 Kaiser Family Foundation, “Employer Health Benets, 2013 Survey,” (August 2013) available at
http://kff.org/private-insurance/report/2013-employer-health-benets/.
NATIONAL WOMEN’S LAW CENTER
4 NEW BENEFITS FOR BREASTFEEDING MOMS NWLC
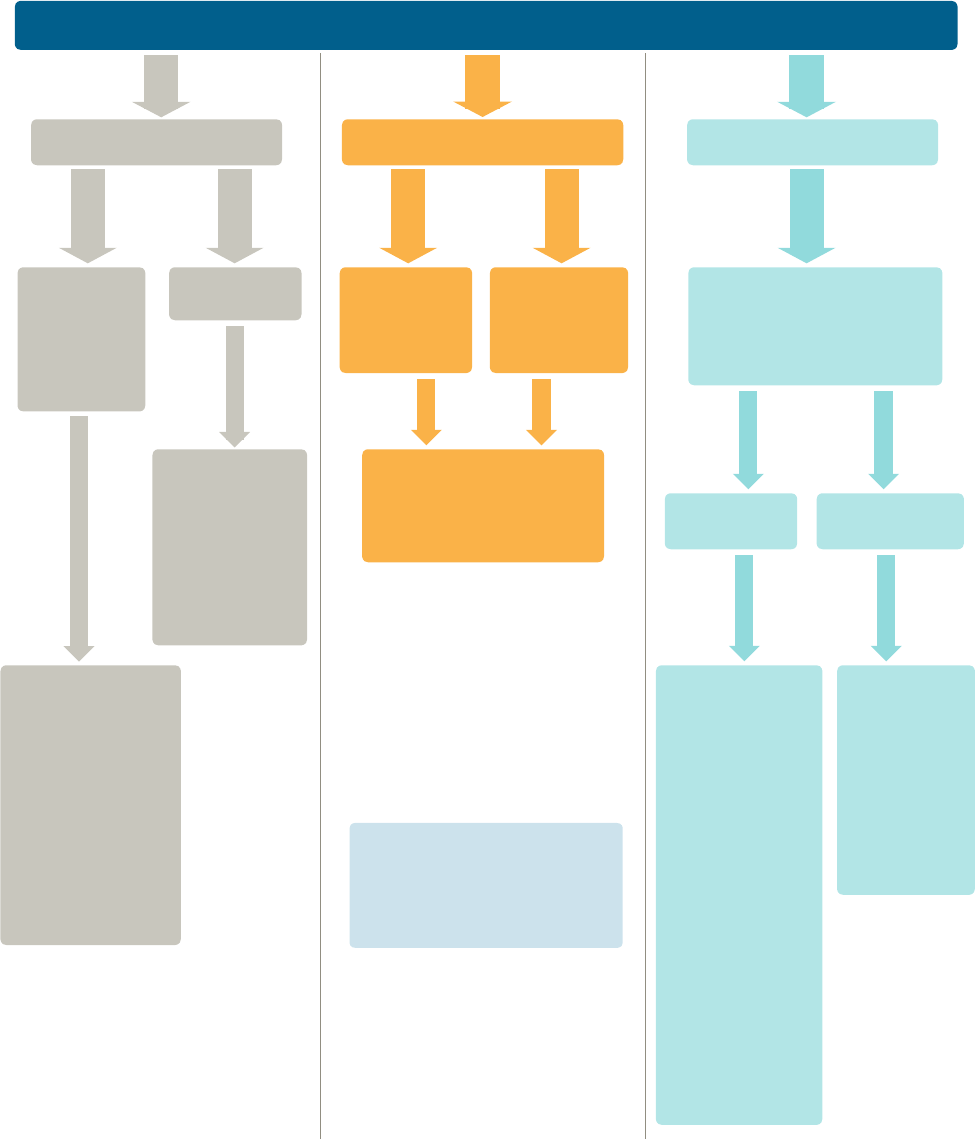
Does my health insurance have to cover breastfeeding supplies
and support without cost-sharing?
What type of health coverage do you have?
Traditional
Medicaid
(including
pregnancy-
related
Medicaid).
Through the
new health
insurance
marketplaces.
Private plan,
not purchased
through the
marketplace.*
YES. All plans
for those newly
eligible for
Medicaid are
required to cover
breastfeeding
support and
supplies.
YES. Non-
grandfathered
plans, or
“new” plans,
are required
to cover
breastfeeding
support and
supplies.
YES. All new private
plans are required to cover
breastfeeding support and
supplies.
Is your plan grandfathered?
(You may have to ask your
HR department or health
insurance company to nd
out.)
MAYBE. In
traditional Medicaid,
coverage of
breastfeeding
support and
supplies varies by
state. These are
considered optional
services and are not
a required part of
coverage.
NO.
Grandfathered
plans are
not required
to provide
breastfeeding
benets. If the
plan makes
signicant
changes (like
decreasing
premiums or
cutting benets),
it will have to
comply with the
requirement.
However, some
plans offer
these benets
voluntarily.
Medicaid
expansion
Grandfathered
Not
Grandfathered
I buy my own insurance Through my jobMedicaid
*If you are enrolled in the same
plan since before March 23, 2010,
your plan may be grandfathered
and would not have to comply with
this requirement.
NATIONAL WOMEN’S LAW CENTER
NWLC NEW BENEFITS FOR BREASTFEEDING MOMS 5
Q: How does coverage of breastfeeding support and supplies t into the
health care law?
A: Under the new health care law, all new health insurance plans must cover certain preventive health services and
screenings without cost-sharing. Breastfeeding support and supplies are one of the preventive services that plans
must cover without any cost-sharing.
Q: Does this mean I won’t have to pay anything for my breastfeeding pump or
lactation consultant?
A: The law requires insurance companies to cover breastfeeding supports and supplies without a copayment or other
cost-sharing. While some plans previously covered these services, many only paid a portion of the cost, while the
woman would have to pay a co-payment or co-insurance. Now, breastfeeding support and supplies will be fully
covered by insurance plans and you will not need to make a separate payment to your healthcare provider or
pharmacy. However, we know that in practice, many women face obstacles in getting their pump or lactation
counseling covered at all, or covered without cost-sharing. If you’re having problems, there are additional
resources in this toolkit to help you.
Q: How do I know if my plan is new and if these requirements apply to
my plan?
A: Health plans that existed before the health care law are considered “grandfathered” into the new system.
Grandfathered plans don’t have to follow the preventive services coverage rules, including providing breastfeed-
ing support and supplies without cost-sharing. This means that the plan can continue to operate just as it has
until it makes signicant changes. These changes include: cutting benets signicantly; increasing co-insurance,
co-payments, or deductibles or out-of-pocket limits by certain amounts; decreasing employer premium
contributions by more than 5 percent; or, adding or lowering annual limits.
Un-grandfathered plans are group health plans created after March 23, 2010, group health plans that have
implemented signicant changes, or individual plans purchased after that date, which is when the health care law
was signed by the President. All un-grandfathered private health plans have to follow the new preventive health
services coverage and cost-sharing rules. When you hear that “all new health plans” have to cover these services,
it means that all “un-grandfathered” plans must cover them.
Questions & Answers:
Breastfeeding Support and Supplies

NATIONAL WOMEN’S LAW CENTER
6 NEW BENEFITS FOR BREASTFEEDING MOMS NWLC
Q: What does “in-network” and “out-of-network” mean?
A: Insurance companies contract with certain providers and facilities that are then considered “in-network” for your
health plan. “Out-of-network” providers are typically not fully covered by your health plan so when you visit an
out-of-network provider you are often responsible for much greater cost sharing or even the whole cost of the visit.
It is important to call your insurance company to verify that the provider you want to see is “in-network.” In general,
in order to obtain your breast pump and counseling at no cost-sharing, you have to go to an in-network provider or
company.
Q: What if my insurance company doesn’t have any lactation consultants or
breast pump supplier in-network?
A: If your insurance company doesn’t have any lactation consultants or breast pump providers in-network, the
insurance company must cover services from an out-of-network provider without cost-sharing. Federal guidance
makes clear that “if a plan or issuer does not have in its network a provider who can provide the particular service,
then the plan or issuer must cover the item or service when performed by an out-of-network provider and not
impose cost-sharing with respect to the item or service.”
1
If your insurance company does not have providers in
its network to provide breastfeeding equipment or lactation counseling, you must be able to go out-of-network, the
item or service must be covered; and covered at no cost-sharing.
Q: Can my insurance company place any limits on my breast pump or lactation
counseling?
A: It depends. Federal regulations make clear that coverage of comprehensive lactation support and counseling and
costs of renting or purchasing breastfeeding equipment extends for the duration of breastfeeding. An insurance
company cannot impose an unallowable waiting period or limit, such as requiring you to obtain the pump within
six months of delivery or limiting the benet to one pump per year. Your insurance company is also not allowed to
refuse to provide lactation counseling or limit this benet to a hospital setting. However, an insurer can use some
limits such as requiring you to rent a pump instead of purchasing one, or requiring you to see an in-network
lactation consultant.
1 Centers for Medicare and Medicaid Services, “Affordable Care Act Implementation FAQs - Set 12,” available at
http://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.html.
NATIONAL WOMEN’S LAW CENTER
NWLC NEW BENEFITS FOR BREASTFEEDING MOMS 7
Calling Your Health Plan:
How to Find Out What Your
Health Plan Covers
If you have private insurance, either through a plan you bought on your own or through your employer, you must rst
determine if your plan is grandfathered or un-grandfathered. (If you have coverage through Medicaid, skip to the last
question.) The best way to nd out if your plan is not grandfathered and if you are entitled to this coverage is to call
your insurance company.
WHO SHOULD I CALL?
We recommend you call the phone number on your insurance card. That number should connect you to customer
service for your insurance company or plan and should have the most up to date information about your health plan.
If you get your insurance through your job, and have an employer-sponsored plan, you may have a benets
administrator you can also ask.
Remember, the person answering the phone is not the person making the decisions. If the person with whom you are
speaking is unable to answer a question you have, you might want to ask to speak with a supervisor. If you do not
believe you are being told correct information and you have insurance through your employer, you may also want to let
your benets administrator know of the issues.
WHAT SHOULD I SAY?
The phone script provided on the next page includes suggested questions you can ask to nd out if your plan is
providing breastfeeding support and supplies, and follow up questions about the details of the coverage. You do not
have to follow the script perfectly. You can use it as a guide.
WHAT IF I HAVE MEDICAID?
Medicaid coverage of breastfeeding support and supplies varies by state. You will probably have to call your state
Medicaid ofce to nd out about coverage. If your annual income is less than 185 percent of the federal poverty level
(about $29,000 for a family of two or $44,000 for a family of four), you can also contact your local Women, Infant, and
Children (WIC) ofce. WIC provides a range of breastfeeding services, including breast pumps, lactation counseling,
and educational materials.
NATIONAL WOMEN’S LAW CENTER
8 NEW BENEFITS FOR BREASTFEEDING MOMS NWLC
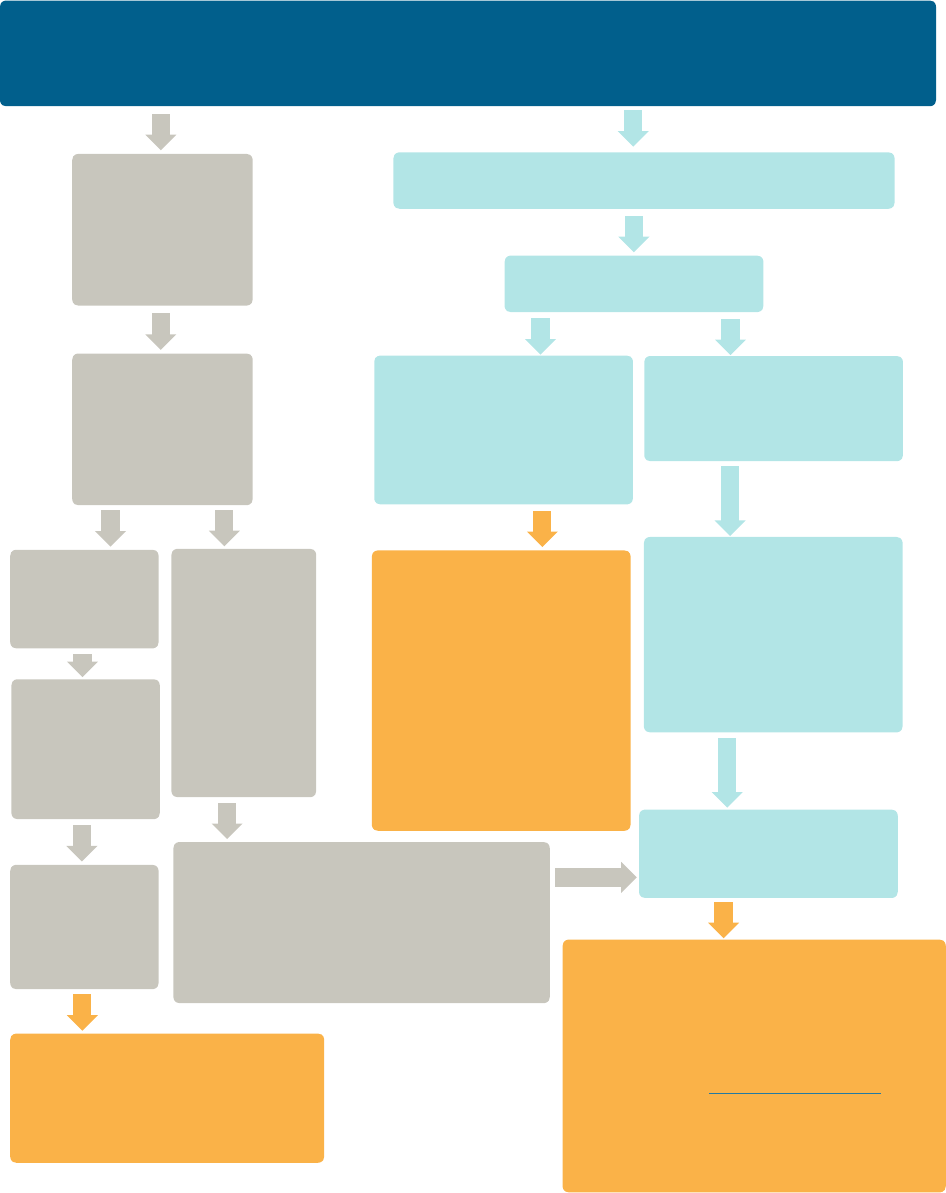
Sample Script:
Calling Your Health Plan
Hi, I understand that under the health care law, all plans are required to cover breastfeeding support
and supplies without cost-sharing. I’m calling to conrm that my plan is covering these services.
Can you tell me if it is?
NO, we don’t cover breast pumps or lactation consultants.
YES, as a new
plan, breastfeeding
supplies and support
are covered without
any cost-sharing.
GREAT! Can you
provide me a list of
in-network lactation
consultants?
YES, our list
can be found
here…
NO, we don’t
have a list of
providers.
You can get
breastfeeding
counseling
through your
pediatrician
or OB/GYN.
THANKS.
And, what is
the process for
getting my
breast pump?
[Most pediatricians or OB/GYNs will not
have a list of providers.] I don’t think my
pediatrician or OB/GYN will have a list, if you
can’t provide a list then I would like to speak
to your supervisor about this policy.
YES, let me
walk you through
that process…
CONGRATULATIONS!
Thanks to the Affordable Care
Act, your plan is covering your
breastfeeding supplies and support.
Is my plan grandfathered?
YES, you’re enrolled in a
plan that began before March
23, 2010 so it doesn’t have to
comply with this requirement.
NO, your plan is not
grandfathered, but we don’t
provide this benet.
Unfortunately, you won’t be
able to get coverage for your
breastfeeding support or
supplies from your current
plan. The plan will have
to comply when it makes
changes such as decreasing
premiums or cutting benets.
The healthcare law requires
that you provide this benet.
Can I speak with a supervisor
to make sure this is the correct
information about this policy?
Repeat these questions to
the supervisor.
If you are still not getting the correct answer,
you have several options:
1. File an internal appeal (see letters at the
end of the toolkit).
2. Contact us at [email protected]
3. If you purchase your plan on your own or
through the marketplace, contact your state
insurance commissioner.
NATIONAL WOMEN’S LAW CENTER
NWLC NEW BENEFITS FOR BREASTFEEDING MOMS 9
PREPARING THE LETTER
• Contact your insurer to nd out to whom you should send your appeal.
• If you are given an appeal form, it will include the address for the person to whom you should send your appeal.
• In addition, if you are in an employer-based plan, you can send a copy of the appeal letter and form to your
insurance plan’s Plan Administrator.
• The contact information for your Plan Administrator can be found in the Summary Plan Description.
• If you are in an employer-sponsored plan and you are comfortable doing so, you should give a copy
to the person who manages employee benets in your HR department.
• Be sure to attach a copy of the “Frequently Asked Questions” to the letter – you can print a copy here:
http://www.dol.gov/ebsa/faqs/faq-aca12.html
• Make a copy of the letter and keep it in your les.
• You can also nd word versions of sample appeal letters here:
www.nwlc.org/breastfeeding
AFTER YOU SEND YOUR LETTER
• Continue to keep copies of receipts or other documents that show when you have had to pay out-of-pocket
for your breast pump or related services.
• Please let us know if you receive a reply from your insurance company. We are keeping track of how
insurers respond.
Sending an Appeal Letter:
Breastfeeding Support and Supplies
IF YOU HAVE ANY QUESTIONS, CONTACT THE NATIONAL WOMEN’S LAW CENTER AT
1-866-745-5487 or [email protected].

NATIONAL WOMEN’S LAW CENTER
10 NEW BENEFITS FOR BREASTFEEDING MOMS NWLC
To Whom It May Concern:
I am enrolled in a [INSURANCE COMPANY NAME] plan, policy number [POLICY NUMBER]. I recently tried to purchase
a breast pump through my health insurance. The Patient Protection and Affordable Care Act requires that my insurance
coverage of this preventive service be with no cost-sharing. However, when I contacted [INSURANCE COMPANY NAME]
about the coverage, I was told I could not get coverage of [BREAST PUMP REQUESTED].
Under § 1001 of the Patient Protection and Affordable Care Act (ACA), which amends § 2713 of the Public Health Services
Act, all non-grandfathered group health plans and health insurance issuers offering group or individual coverage shall
provide coverage of certain preventive services for women with no cost-sharing. The list of women’s preventive services
which must be covered in plan years starting after Aug. 1, 2012 includes “comprehensive lactation support and counseling
and costs of renting or purchasing breastfeeding equipment [] for the duration of breastfeeding” (see attachment).
My health insurance plan is non-grandfathered. Thus, the plan must comply with the women’s preventive services.
[INCLUDE THIS PARAGRAPH IF YOUR PLAN DOES NOT HAVE A CLEAR PROCESS TO GET A PUMP]
My health care provider has prescribed that I use [BREAST PUMP REQUESTED]. The insurance plan has not established
a process for me to obtain a pump, such as through a durable medical equipment supplier, and thus it remains an
over-the-counter product for the purposes of my plan. As the FAQs on the preventive services (dated February 20, 2013)
state, “OTC recommended items and services must be covered without cost-sharing…when prescribed by a health care
provider.” Accordingly, [INSURANCE COMPANY] must cover [BREAST PUMP REQUESTED] as required under the
Affordable Care Act.
LAST PARAGRAPH OPTIONS:
(1) I have spent [TOTAL AMOUNT] out-of-pocket on [NAME OF BREAST PUMP], despite the fact that it should have been
covered. I have attached copies of receipts which document these out-of-pocket expenses. [COMPANY NAME] must
rectify this situation by reimbursing me for the out-of-pocket costs I have incurred during the period it was not covered
without cost-sharing. Furthermore, [COMPANY NAME] must ensure breastfeeding support and supplies, including lactation
counseling are covered without cost-sharing in the future by changing any corporate policies that do not comply with the
Affordable Care Act.
(2) I am prepared to order [BREAST PUMP REQUESTED] when [COMPANY NAME] assures that I have coverage without
cost-sharing. I expect that [COMPANY NAME] will rectify this situation and notify me within 30 days of receipt of this letter
that [BREAST PUMP REQUESTED] will be covered without cost-sharing.
Sincerely,
[YOUR SIGNATURE]
Encl:
Frequently Asked Questions about the Affordable Care Act (Part XII), available online at
http://www.dol.gov/ebsa/faqs/faq-aca12.html)
Copies of Receipts Documenting Out-of-Pocket Costs
Sample Letter:
No Coverage Policy for Breast Pump

NATIONAL WOMEN’S LAW CENTER
NWLC NEW BENEFITS FOR BREASTFEEDING MOMS 11
To Whom It May Concern:
I am enrolled in a [INSURANCE COMPANY NAME] plan, policy number [POLICY NUMBER]. I recently tried to
access lactation counseling that should be covered by my health insurance. The Patient Protection and Affordable
Care Act requires insurance coverage of breastfeeding support and supplies with no cost-sharing. However, when I
contacted [INSURANCE COMPANY NAME] about the coverage by [SPECIFY METHOD, PHONE] on [DATE], I was
told I could not get coverage of [LACTATION COUNSELING] because [SPECIFY REASON, SUCH AS NO
IN-NETWORK PROVIDERS].
Under § 1001 of the Patient Protection and Affordable Care Act (ACA), which amends § 2713 of the Public Health
Services Act, all non-grandfathered group health plans and health insurance issuers offering group or individual
coverage shall provide coverage of certain preventive services for women with no cost-sharing. The list of women’s
preventive services that must be covered in plan years starting after Aug. 1, 2012 includes “comprehensive lactation
support and counseling and costs of renting or purchasing breastfeeding equipment [] for the duration of breastfeeding”
(see attachment).
My health insurance plan is non-grandfathered and the plan year started on [PLAN YEAR DATE]. Thus, the plan must
comply with the women’s preventive services provision.
The insurance plan has not established a process for me to obtain in-network lactation counseling, as required by
federal law. Federal guidance on the preventive services clarify that, “… if a plan or issuer does not have in its network a
provider who can provide the particular service, then the plan or issuer must cover the item or service when performed
by an out-of-network provider and not impose cost-sharing with respect to the item or service.”
Since [PLAN YEAR DATE], I have spent [TOTAL AMOUNT] out-of-pocket on [LACTATION COUNSELING], despite
the fact that it should have been covered during that time. I have attached copies of receipts which document these
out-of-pocket expenses. [COMPANY NAME] must rectify this situation by reimbursing me for the out-of-pocket costs I
have incurred during the period it was not covered without cost-sharing. Furthermore, [COMPANY NAME] must ensure
breastfeeding support and supplies, including lactation counseling are covered without cost-sharing in the future by
changing any corporate policies that do not comply with the Affordable Care Act.
Sincerely,
[YOUR SIGNATURE]
Encl:
Frequently Asked Questions about the Affordable Care Act (Part XII), available online at
http://www.dol.gov/ebsa/faqs/faq-aca12.html)
Copies of Receipts Documenting Out-of-Pocket Costs
Sample Letter:
Coverage for Lactation Consultant

11 Dupont Circle, Suite 800
Washington, DC 20036
202.588.5180 | fax 202.588.5185
www.nwlc.org
